It was my tour on the medic unit. When I arrived to work the paramedic from the previous shift was restocking the ALS bag, they looked exhausted. “Bad dope in town” they muttered. By mid-afternoon I had used as many narcan (naloxone) vials as fit in a front pants pocket. This was heroin mixed with “something” and people in this Mid-Atlantic region were “dropping like flies.” The landscape today is markedly different, but it’s built on years of opioid use and abuse, from pain medications to heroin. Now, as responders, planners, managers, and leaders, we have to worry not only about the overdose victim(s) but our first responders who arrive to assist. If you follow HSIN, EMR-ISAC, and the CDC, you likely noticed increased mention of fentanyl and various derivatives or analogs. These chemicals and mixtures are so potent and deadly that we are at risk of injury ourselves, not to mention their potential as WMD or incapacitating agents.
The example above was challenging nearly ten years ago and yet it somehow still seemed routine. Today, there is a new class of drugs that poses a challenge to ALL responders that should serve as a paradigm shift. Illicit drug use can now significantly and fatally affect the responders through skin contact (absorption) or inhalation. Fentanyl and its analogues (acrylfentanyl, sufentanil, carfentanil, etc.) are being used alone or mixed with other drugs for illicit use and the rate and impacts are alarming.13 Compounding the problem is that carfentanil and other analogs are readily available.6,7
A GRAIN OF SALT
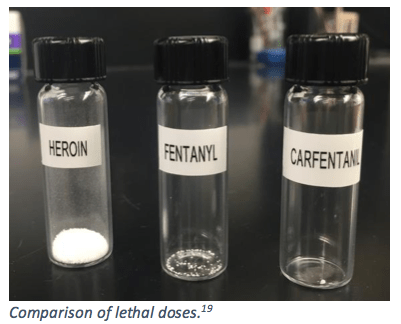
Morphine is a commonly used/prescribed opioid pain management medication both in and out of clinical settings. Stronger than morphine, fentanyl is a prescribed opioid pain management medication and comes in various forms, from injectable solutions to patches to lollipops. Stronger still is carfentanil, also an opioid and an analogue of fentanyl that was developed for large-animal sedation.2 Some common synonyms are: carfentanyl, Wildnil, 4-carbomethoxyfentanyl.2 For the sake of comparison, fentanyl is 100 times STRONGER than morphine, used when a more powerful pain management medication is needed for those already accustomed to the effects of less potent opioid medications. 15 Carfentanil is up to 100 times stronger than fentanyl and 10,000 times stronger than morphine.3
Formulas and Potency:2, 17
| NAME | FORMULA | POTENCY (compared to morphine) |
| morphine | C17H19NO3 | 1 |
| heroin | C21H23NO5 | 2 |
| fentanyl | C22H28N2O | 100 |
| carfentanil | C24H30N2O3 | 10,000 |
The CAS for carfentanil is 59708-52-0 with a PubChem ID of 62156 and it is listed as a poison.2 It can be found in numerous forms, including: powder, spray, blotter paper, and tablets. It is white when pure, however it takes on other colors when it is mixed with other chemicals, such as heroin, often in the range of browns or tans.3 Routes of exposure vary and include absorption, inhalation, ingestion, and injection.3 The greatest concern for responders will be the first two, absorption and inhalation. Due to the extreme level of toxicity, an incredibly small amount inhaled or absorbed can cause rapidly evolving symptoms.
As an estimation of the mass of a single grain (piece) of salt consider the atomic masses of sodium and chlorine and estimate the size (at least an average) of a single piece of salt. The result is approximately 58.5 ug (micrograms.) 18,19 The human threshold of carfentanil is 1 microgram and 20 micrograms is considered a fatal dose.2 In other words, the amount of pure carfentanil that can kill a person is smaller than the average grain of salt. A grain of SALT!
NORMAL ISN’T NORMAL
Overdose incidents were once considered “normal” in pre-hospital EMS. In fact, the definition of “normal” has changed so much that what was once an Advanced Life Support skill (Narcan administration) is performed at the Basic Life Support level. Furthermore, law enforcement now often carries Narcan for the reversal of an opioid overdose without EMS involvement. The prevalence of opioids for illicit use has turned these life-threatening incidents into routine responses for the medical profession simply because they are so common. Today, that has all changed. A relaxed mindset of “just an overdose” or an “EMS-only response” is what has gotten several emergency responders extremely sick treating these new overdose patients. It is important to note that this is not necessarily due to complacency by the responders, but normal isn’t normal anymore and the unexpected is leaning towards routine. Fentanyl and its analogs are readily available and they are often mixed with other illicit drugs, potentially unknown to the user. The evidence shows a marked increase in overdose deaths over the past several years due to these opioids and the trend is now clearly indicating that responders are falling victim at an alarming rate as well. 6,7,8,12,13,23
The symptoms are still the same as other opioid overdoses. Patients present rapidly with an altered or decreased level of consciousness, respiratory depression, and pinpoint pupils.3,23 These symptoms can occur quickly, within minutes, with effects building over the course of hours for inhaled or absorbed contamination.11 Typical treatment, as mentioned, has been the use of Narcan. For a once “typical” opiate overdose, such as heroin, the normal dose of Narcan is up to 2.0 mg. Although Narcan works, fentanyl and its analogs are MUCH too strong for single-dosing to be effective. Here’s why… Narcan has a half-life of 30-81 minutes, significantly shorter than those of the basic opioids such as morphine or heroin, which are in the range of 2.0-3.5 hours. Now take fentanyl, this has a half-life of 3.7 hours and carfentanil 7.7 hours.21,22 What this means is that the Narcan STOPS WORKING long before the opioid has been removed from the system allowing the opioid a chance to re-bind, causing the overdose to reoccur. This is part of the reasoning behind the need for multiple administrations of Narcan for fentanyl and analog overdose victims.4,23
WMD
Up to this point, we have discussed the rise of fentanyl and now carfentanil use in the US as an illicit drug and its effects on first responders. By taking a slightly different point of view, there is another arena where these drugs can be concerning for the entire response community, again from responder to the planners and managers. There is some belief that carfentanil was used specifically as an incapacitating agent by the Russian military in 2002 during the Dubrovka Theater in Moscow.25 Numerous fatalities resulted and the methods for reversal proved too little, too late for many of them. Due to the extreme toxicity, availability, and routes of exposure, there is a valid possibility of carfentanil (or any of the fentanyls and analogs) use as a WMD agent. From dispersal methods involving ANY route of entry, only a TINY amount is required. For example, a recent 1kg discovery of carfentanil in Canada could potentially be considered 50 million fatal doses.31 (For reference, 1kg is equal to 2.2 pounds and the population of New York City is less than 10 million people.)
For the sake of comparison, fentanyl is 100 times STRONGER than morphine, used when a more powerful pain management medication is needed for those already accustomed to the effects of less potent opioid medications. 15 Carfentanil is up to 100 times stronger than fentanyl and 10,000 times stronger than morphine.3
RESPONSE
Education, training, and interoperability are key to the safe mitigation of these incidents. Personnel at all levels of response-authority must be educated on the dangers of these new drugs, and aware that more and more analogs may be developed. The concern isn’t just the single overdose victim and incident scene, but the potential for WMD use and special considerations that need to be made for recognizing, responding, and mitigating these incidents. Remember, “normal isn’t normal” anymore. Proper training needs to be developed and disseminated that is based on best-practices and lessons learned. These are FUSION incidents. Law enforcement, HazMat, fire, and EMS are likely the first to encounter these incidents. Law enforcement and EMS personnel have already been injured by encountering fentanyl and carfentanil in the field and many law enforcement agencies have stopped the field-screening process of unknown powders completely.23,24,31 It is imperative that we develop strong relationships with our response partners and intelligence community to rapidly identify and foster interoperability relationships.
So how do we respond to these incidents? The following section will cover some of recommendations developed by Federal agencies in coordination with state and local response partners.
Scene Identification
One of the greatest challenges with these incidents is that there are few marked identifiers. These incidents can occur ANYWHERE and at ANY TIME, and can be seen as a single “unconscious person” to a large number of incapacitated or unconscious persons. Since carfentanil is commonly found in street drugs, there is now another layer of hazard associated with clandestine lab incidents. Always assume that until determined otherwise, the product is of the highest toxicity.
A hazard and risk assessment is essential. If the hazard of a fentanyl or analog is suspected, the hazard is high. At that point the risk to life, property, and environment can be identified. If there is any suspicion of the presence of fentanyl or an analog, evaluate the risk to yourself, other responders, and the public. Notification and resource requests should be made quickly and only those personnel properly trained and equipped for identifying and handling these chemicals should be allowed in the area. 9 Additionally, recognize the signs of exposure as discussed above, including altered or decreased level of consciousness, respiratory depression, and pinpoint pupils.3,23 Establish hazard control zones quickly and secure them.
Carfentanil
- Synthetic opioid, analog of fentanyl
- 10,000 times stronger than morphine
- Color: white to range of browns/tans, typically as solids or liquids
- Symptoms: Altered level of consciousness, respiratory depression, and pinpoint pupils
- Treatment: Narcan/naloxone. Multiple doses
- Routes of exposure: Inhalation, absorption, ingestion, injection
- Response: Unified command, multi-agency
- CPC/PPE: Highest level of skin and respiratory protection, redundancy of instrumentation
- Decontamination: Soap and water, brush agitation
Carfentanil Synthetic opioid, analog of fentanyl 10,000 times stronger than morphine
Incident Command
This will be a Unified Command event, involving personnel from multiple agencies and/or jurisdictions. Although these drug-related incidents appear to be solely for law enforcement, there is a major HazMat nexus for the response and mitigation. It cannot be stressed enough that relationship development must happen BEFORE an emergency. The incident scene is not the time to learn how one works with their response partners. Develop a command structure early that can incorporate these agencies and allow for a modular expansion as needed. At the very least consider an incident commander (or Branch/Division Chief) with HazMat experience, a safety officer, EMS for patients/victims AND responders including Advanced Life Support, decontamination (including emergency-use), an entry/recon team, and a backup/RIT team. Additional groups could include a forensics group and research group. This level of response may not be needed on EVERY potential overdose victim, but if your hazard/risk analysis suggests unknowns and there is a high index of suspicion, be prepared to build-out a formal response framework.
Personal Protective Equipment11
This is information specific to FENTANYL, however, the significantly increased potency of the fentanyl analogs, including carfentanil, erring on the side of caution is certainly warranted. Due to the multiple routes of exposure (inhalation, ingestion, absorption) and extreme toxicity consider a Level A entry. This includes a fully-encapsulating CBRN suit with SCBA, inner and outer gloves (nitrile recommended,) and “chemical resistant” boots.
Decontamination11
The basics of decontamination apply: uphill and upwind. Decontamination should be performed with a soap and water solution, using brushes for agitation. The corridor should capture the decontamination solution with concern given to the protection of storm drains, sewers, and water sources such as streams and ponds. Since there is little information available about further definitive methods of decontamination, this is another case where being overly cautious might be the best approach.
Instrumentation
Until quite recently field testing of drugs was routinely performed by law enforcement. The nature of these new opioids has necessitated procedural changes at the field level with many organizations preventing law enforcement testing of unknown powders in the field. 24,31 Since these incidents can and should involve HazMat personnel, there are some go-to instruments that can be used to identify unknowns. As with any unknown, entry should be made to identify the presence of the following: Radiation, pH, flammability (CGI, PID), oxygen (enriched or deficient), and toxicity (KI paper, F paper, M8 paper, M9 tape, PID, multi-gas.) Once those hazards have been ruled in or out and mitigated, specific and focused reconnaissance can be performed with some specialized instrumentation many HazMat teams possess already. Of particular importance is the concept of redundancy. Although a particular instrument may indicate the presence (or absence) of “something” utilizing one or two additional devices as confirmation is quite important. Despite the advances in field diagnostic tools, utilizing a state-level forensic laboratory or a Laboratory Response Network (LRN) facility should be considered to provide definitive results.
Besides law enforcement’s field screening kits, there are advanced technologies that can be utilized to identify these compounds. RAMAN, FTIR, and Mass Spectrometry are three commonly used devices in the field that are all successful with opioid identification. Each also offers “reachback” support for non-library items, a benefit for “unknown” instrument responses to samples. Additional information can be found regarding these and other technologies via manufacturer websites. An example of each is included below, without endorsement of the manufacturer or technology.
RAMAN
Recent Developments in Handheld Raman Spectroscopy – click for link.
Quick ID of Opioid-Containing Drugs White Paper – click the link for pdf.
FTIR
HazMat ID by Smiths
Mass Spectrometry
Q&A with John Kenneweg – The Changing Threat Landscape
908 Devices
CONCLUSION
The threat landscape changes as rapidly as it is learned and understood. Seemingly typical or “normal” incidents even just a few years ago are being replaced by extremely hazardous and risky events for responders. There is no normal anymore as the shift towards stronger opioids poses a monumental challenge to responders and planners. Carfentanil is more than just an add-on to typical street drugs and its potential as a WMD is alarming. Drug users are dying, responders are getting extremely sick, and as a response community, regardless of level, we must be prepared to respond to and mitigate these incidents. Interoperability is a crucial component. Strong, working relationships with response partners must be developed prior to the emergency scene. This facilitates smoother incident operations due to the joint-hazard nature of these incidents. There are a myriad of response tactics that can and should be employed, from selection of CPC and instrumentation, to defined roles of the command structure and inter-agency training.
Be safe and be smart.
END NOTES
- https://chem.nlm.nih.gov/chemidplus/sid/0059708520 Accessed 20 April 2017.
- https://pubchem.ncbi.nlm.nih.gov/compound/carfentanil Accessed 20 April 2017.
- https://www.drugs.com/illicit/u-47700.html Accessed 20 April 2017.
- https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/AnestheticAndAnalgesicDrugProductsAdvisoryCommittee/UCM524338.pdf Accessed 20 April 2017.
- https://canadiancentreforaddictions.org/carfentanil-dangers/ Accessed 20 April 2017.
- https://www.dea.gov/docs/Counterfeit%20Prescription%20Pills.pdf Accessed 20 April 2017.
- http://www.npr.org/sections/health-shots/2016/09/02/492108992/an-even-deadlier-opioid-carfentanil-is-hitting-the-streets Accessed 20 April 2017.
- https://manchesterinklink.com/carfentanil-weapon-community-war/ Accessed 20 April 2017.
- https://www.dea.gov/divisions/hq/2016/hq092216_attach.pdf Accessed 20 April 2017.
- http://pittsburgh.cbslocal.com/2017/04/28/narcan-resistant-fentanyl-pennsylvania/ Accessed 24 April 2017.
- https://www.cdc.gov/NIOSH/ershdb/EmergencyResponseCard_29750022.html Accessed 24 April 2017.
- http://www.economist.com/news/leaders/21722189-criminalisation-not-right-way-approach-it-or-other-drugs-fentanyl-next-wave?fsrc=scn/FB/te/bl/ed/ Accessed 24 April 2017.
- http://www.economist.com/news/briefing/21722164-legal-highs-fentanyl-there-are-more-drugs-offer-ever-expanding Accessed 24 April 2017.
- http://www.tandfonline.com/doi/full/10.1080/15563650.2016.1217003?scroll=top&needAccess=true (excerpt from Clinical Toxicology “New Psychoactive Substances (NSP) – the hydra monster of recreational drugs” Accessed 24 April 2017.
- http://www.narconon.org/drug-information/fentanyl.html Accessed 24 April 2017.
- https://www.drugabuse.gov/about-nida/directors-page/messages-director/2006/06/fentanyl-use-in-combination-street-drugs-leading-to-death-in-some-cases Accessed 25 April 2017.
- http://www.kgw.com/news/fentanyls-deadlier-cousin-a-few-grains-of-carfentanyl-can-kill/296315308 Accessed 25 April 2017.
- http://www.physlink.com/Education/AskExperts/ae342.cfm Accessed 25 April 2017.
- http://www.bluebulbprojects.com/measureofthings/singleresult.php?comp=weight&unit=kgms&amt=3.0E-7&i=363 Accessed 25 April 2017.
- http://nhpr.org/post/first-responders-prepare-possible-surge-deadly-carfentanil-use-nh#stream/0 Accessed 25 April 2017.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2704132/ Accessed 25 April 2017.
- http://www.rxlist.com/narcan-drug/clinical-pharmacology.htm Accessed 25 April 2017.
- http://www.jems.com/articles/2016/12/carfentanil-exposure-treatment-precautionary-measures-for-ems-providers.html Accessed 25 April 2017.
- http://circa.com/scitech/health/fentanyl-is-so-strong-its-putting-first-responders-at-risk-just-by-touching-it Accessed 25 April 2017.
- http://www.bbc.com/news/world-europe-20067384 Accessed 5 May 2017.
- http://www.spectroscopyonline.com/recent-developments-handheld-raman-instrumentation-industry-pharma-police-and-homeland-security-532 Accessed 5 May 2017.
- http://pittcon.org/wp-content/uploads/2017/01/BIOTOOLS_Opioids_White_Paper.pdf Accessed 5 May 2017.
- https://www.smithsdetection.com/index.php?option=com_k2&view=item&id=102&Itemid=101#.WSa5oevyvcs Accessed 5 May 2017.
- http://908devices.com/blog/qa-john-kenneweg-changing-threat-landscape/ Accessed 5 May 2017.
- http://www.officer.com/article/12263320/dea-warning-to-law-enforcement-fentanyl-and-carfentanil-exposure-kills Accessed 5 May 2017.
- https://www.fentanylsafety.com/wp-content/uploads/OPIOID-MISUSE-INTERIM-GUIDANCE_2.pdf Accessed 5 May 2017.

About the Author
David (Dave) Millstein
David (Dave) Millstein has been involved in the emergency services since 2000 as a volunteer in Pennsylvania and since 2004 with Frederick County (MD) Fire/Rescue. Outside of the fire department, he worked for the USFA supporting the NFIRS system and as a HazMat contractor in the Mid-Atlantic region. Originally from Massachusetts, he stayed in Pennsylvania for his career. Dave’s passion is focused on leadership and management in the area of HazMat/WMD, including planning, leadership, and management to prepare personnel for current and future threats/hazards. He is currently pursuing a MS in Emergency Management. When he is not working, he enjoys hiking with his family, Tae Kwon Do, reading, and writing.